Abstract
Background: Primary Bone Lymphoma (PBL) is recognised as an uncommon subtype of lymphoma exclusively affecting bone tissue, however limited data is available regarding its clinical features, optimal treatment approach and outcomes.
Methods: A retrospective review of all patients with PBL treated at Princess Margaret Hospital from January 1st, 2000 to December 31st2020 was performed. Information regarding clinical presentation, histological subtype, prognostic factors, treatment, disease response and survival were collected. Primary bone lymphoma was defined as confirmed histological diagnosis of lymphoma affecting bone as primary site of disease. Cases with non-contiguous disease were excluded. At the end of treatment, disease response was assessed by combination of computed tomography, bone scintigraphy, magnetic resonance imaging (MRI) and positron emission tomography as per era-specific practices.
Results: A total of 87 patients were identified, with a median age of 54 years (17 - 90) of which 61% (n= 53) were male. Median follow up time was 5.8 years (0.2-20.1). The majority (68.9%) had a good performance status at diagnosis (Eastern Cooperative Oncology Group ECOG status of 0-1) and 55.2% (n=48) presented with axial disease alone, 33.3% (n=29) had appendicular disease alone, and 11.5% (n=10) had both. According to Ann Arbor staging criteria, 62.0% (n=54) of patients had stage IE disease, 13.7% (n=12) patients had stage IIE disease (single bony site with contiguous/closely associated nodal disease), and 24.1% (n=21) patients had stage IV disease (multifocal bone disease). International prognostic index (IPI) were available for 82 patients, with 17.6% with IPI-0, 32.9% with IPI-1, 25.9% with IPI-2, 14.1% with IPI-3, and 5.9% with IPI-4. Thirteen percent (n=11) of patients had spinal cord compression at diagnosis and 18.4% (n=16) had a pathological fracture. Bulky disease, defined as greater than 10cm, was seen in 10.3% (n=9) of patients. Histological subtypes included diffuse large B cell lymphoma (88.51%), high grade B cell lymphoma (3.45%) and 8% had an unclassifiable high grade B-cell subtype.
The majority of patients (79.1%) were treated with combined modality therapy, and all patients who received chemotherapy were treated with an anthracycline-containing protocol. Eighteen patients (20.9%) received chemotherapy alone, and one patient was treated with radiation alone. Sixty-seven patients (79.3%) received rituximab. Eighteen (20.6%) patients required initial surgical intervention. Of the patients with Stage IV disease, 47.6% received chemotherapy and radiotherapy, with two of these cases for acute spinal cord compression. Seventy-two (82.7%) achieved a complete response, 5 (5.7%) partial response, 1 (1.1%) stable disease, and 5 (5.7%) patients had progressive disease. Of the patients who responded, 8 (9.1%) patients experienced relapsed disease and went on to salvage treatment. All but one patient relapsed at a different site/s of disease than at diagnosis.
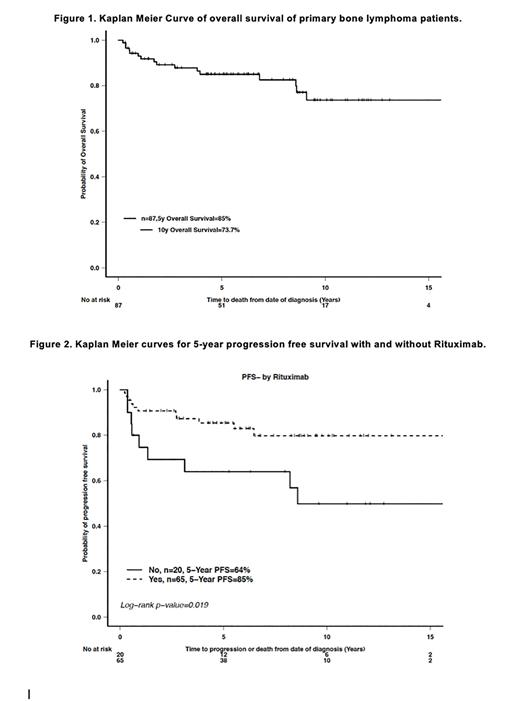
Five-year and 10-year overall survival (OS) and progression free survival (PFS) rates were 85% and 73.7%, and 80.3% and 71.1%, respectively (Figure 1). The 5 year PFS for those treated with Rituximab was 85%, compared with 64% for those treated without (p=0.019), and the 5-year OS for the rituximab group was significantly higher (Figure 2). Those with spinal cord compression had 5 year OS of 55%, compared with 90% in those without (p=0.033). Patients with poor ECOG status also had reduced 5 year OS (ECOG 0-2: 88%, ECOG 3 or more: 50%, p=0.003). Interestingly, there was no difference in the 5 year OS seen dependent on IPI or age. The difference in the 5 year PFS in those treated with a combined modality approach (85%) and those treated with chemotherapy alone (67%) did not reach statistical significance (p=0.053). On univariable Cox regression analyses, ECOG performance status, spinal cord compression and use of rituximab was found to significantly impact upon OS, whereas, age <= 60, ECOG performance status of 0 to 2, IPI score of 0 to 3, axial or appendicular involvement but not both, and rituximab use was found to impact favourably upon PFS.
Conclusions: Primary bone lymphoma is an uncommon disease entity with good survival outcomes when treated with a combined modality approach, although the utility of radiation in the rituximab era would need to be confirmed with a larger study.
Disclosures
Crump:Roche: Research Funding; Kyte-Gilead, Novartis: Honoraria. Kridel:Abbvie: Research Funding. Kukreti:Kwoya Kirin: Honoraria; EUSA Pharma: Honoraria. Prica:Astra-Zeneca: Honoraria; Kite-Gilead: Honoraria.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal